Am I at risk of having a heart attack?
12 October 2017 / 10:40 am

Heart attacks remain the single commonest cause of death in the British Isles and although death rates are reducing there are still many ways that the population can help protect themselves. It is believed that 90% of premature cardiac events are preventable by simple (and free) lifestyle changes, most particularly not smoking, exercising more and losing weight.
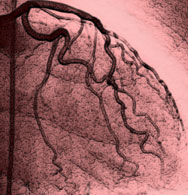
The heart has a large muscle with three main blood vessels supplying oxygen rich blood to it. When we exercise the heart needs more blood to reach it to cope with the extra energy requirements of a faster heartbeat.
As we get older many of us develop fatty deposits or atherosclerotic plaques in the walls of our blood vessels. This process occurs slowly and is believed to be controlled by a repeated process of inflammation and healing. The plaques are made of up cholesterol rich fats covered by a fibrous cap. Atherosclerosis is more common with increasing age, in smokers, in people with diabetes, high blood pressure, those with a sedentary lifestyle, a family history of heart disease and physical inactivity. Emotional and dietary stressors such as oxidants may have a role to play.
A heart attack is caused by a sudden reduction in blood supply to the heart. A typical heart attack occurs when the fibrous cap of a plaque ruptures, allowing the blood access to the fatty core of the plaque. The body tries to heal this by creating a clot that can suddenly reduce the flow of blood to the heart causing symptoms such as chest pain. If the blood vessel is blocked completely then parts of the heart muscle will not get adequate blood supply causing damage to the tissues and a heart attack. Other causes of heart attacks include embolism or passage of clots around the body into one of the heart arteries or a sudden tear or spontaneous dissection of a heart artery.
The treatment of a heart attack therefore is to attempt to limit the amount of damage to the heart muscle by rapidly removing or dissolving the blockage in the artery. This is usually performed with clot busting drugs or mechanical treatments such as angioplasty and stents.
So how can you find out if you are at risk? If you are over forty and haven’t seen your General Practitioner for a long time then please make an appointment to see them to talk about your cardiovascular risk profile. Simple online tools such as QRisk allow a calculation of 10-year likelihood of having or developing heart disease and the impact and effectiveness of interventions. Medical treatment with statins in the right population group makes a significant difference in reducing event rates. Cardiac screening techniques such as the Gold package from Heart for Life as well as CT cardiac calcium scoring can provide more accurate personalised risk assessment when needed. Your GP can help you choose the right tests.
Finally never ignore warning symptoms from your chest. Most heart attacks involve central chest pain lasting more than a few minutes but pain can fluctuate in duration and severity. Sometimes it is squeezing or tight and the pain can radiate to the jaw, teeth, arm or through to the back. If you have chest pain that continues then please call 999 and seek medical assistance.
More Posts
16 March 2024
Developing a new strategy for healthy Islanders
4 February 2024
A digital health diary for Jersey
27 December 2022
Utilising artificial intelligence in cardiology practice
12 June 2022
Under the bonnet – time for your heart’s MOT
12 March 2022
What is heart valve disease and what does that mean for me?
12 January 2022
Preventing heart disease using augmented digital health intelligence
1 October 2021
How heart health has been impacted by COVID-19
1 August 2021
The importance of the rhythm of your heart
21 June 2020
What is atrial fibrillation?
8 April 2020
Coronary heart disease and risk of heart attacks
11 January 2020
The Era of Immersive Health Technology
22 September 2019
The heart and stress
18 August 2019
Screening for Atrial Fibrillation and the Role of Digital Health Technologies
20 November 2018
Ectopic beats – how many count?
28 July 2018
How can immersive VR and AR technologies improve your physical and mental health?
7 March 2018
“The patient takes charge” – enhanced care with Digital Health technologies